Chronic Diseases Now Account for 75% of Deaths Globally
Chronic diseases have become the leading cause of death and disability worldwide. Noncommunicable diseases, such as heart disease, cancer and diabetes, kill 41 million people every year, amounting to 74% of deaths globally. In the U.S., these conditions account for 8 out of the top 10 causes of death.

The shift from infectious diseases to chronic, noncommunicable ailments began in the early 1900s, driven by improvements in sanitation, nutrition and medical technology. However, this transition has come with its own set of challenges. As the population ages and lifestyles change, the prevalence of chronic diseases continues to climb.
The cost to health systems is staggering — over $1 trillion annually in the U.S. alone. Fortunately, there are many steps you can take to lower your risk and prevent chronic diseases. Understanding effective prevention strategies is essential for improving your overall health and well-being.
The Big Four: Heart Disease, Cancer, Diabetes and Dementia
Among chronic diseases, four stand out as particularly impactful: heart disease, cancer, diabetes and dementia. Heart disease remains the leading cause of death in the U.S. Cancer follows closely behind, claiming over 600,000 lives annually. Diabetes affects more than 37 million Americans, with millions more undiagnosed or living with prediabetes.
Alzheimer’s disease and other forms of dementia are rapidly growing concerns, with an estimated 6.7 million Americans aged 65 and over currently affected. These conditions not only impact your health and longevity but also place an enormous financial burden on individuals and health care systems.
The global cost of cancer alone is projected to reach $25 trillion between 2020 and 2050, with five cancers — tracheal, bronchial and lung; colon and rectal; breast; liver and leukemia — accounting for nearly half of that cost. As these diseases become increasingly prevalent, prevention and early intervention to protect your health and quality of life is crucial.
Most Americans Suffer from Chronic Disease
Close to 60% of U.S. adults have at least one chronic disease. About 40% suffer from multiple chronic conditions. A recent study published in Frontiers in Public Health has also projected a significant increase in chronic diseases among adults aged 50 and older.
By 2050, the number of Americans in this age group is expected to surge by 61%, reaching 221 million. Further, those with at least one chronic condition are projected to increase by 99.5%, from 71.5 million in 2020 to 142.7 million by 2050.
Researchers considered nine major chronic conditions, including high blood pressure, diabetes, cancer, chronic lung diseases, heart disease, stroke, arthritis and psychiatric problems. These projections highlight the urgent need for you to take proactive steps in managing your health, as the likelihood of developing a chronic condition increases with age.
The Rise of Multimorbidity: A Growing Concern for Your Health
While the increase in single chronic conditions is concerning, the rise in multimorbidity — having two or more chronic conditions — is equally worrying. The study predicts a 91.1% increase in multimorbidity cases, from 7.8 million in 2020 to 14.9 million by 2050.
The majority of people with chronic conditions or multimorbidity are between 60 and 79 years old. However, the most significant increase is projected for those 80 and older, with a staggering 244% rise in single chronic conditions and a 202.7% increase in multimorbidity cases from 2020 to 2050.
The study also reveals interesting patterns in chronic disease distribution across gender and racial lines. By 2050, women are projected to make up 53% of those with a single chronic condition, while men will form the majority (51%) of those with multimorbidity. Among racial groups, non-Hispanic Whites are expected to see the largest increase in absolute numbers, but other racial groups will experience significant rises as well.
For instance, the number of Hispanics with at least one chronic condition is projected to increase by 110% from 2020 to 2050. These disparities highlight the need for targeted health interventions and personalized approaches to chronic disease prevention and management.
Understanding your own risk factors based on your gender and racial background will help you take more effective steps to prevent chronic disease. However, adopting a holistic approach to your health, addressing not just individual symptoms but the underlying causes of disease, is essential for everyone, at all life stages.

Geographic Patterns of Chronic Disease
Your risk of chronic disease isn’t just influenced by individual factors — it’s also closely tied to where you live. Research published in Preventing Chronic Disease unveiled geographic patterns in chronic disease prevalence across the U.S.
The southeastern region of the country stands out as a hotspot, with clusters of high chronic disease prevalence throughout. This pattern isn’t random; it reflects decades of social and economic policies that have created environments conducive to poor health outcomes.
In contrast, areas with lower chronic disease prevalence are more scattered, often clustering around major metropolitan areas. For instance, in Texas, you’ll find pockets of lower prevalence around Dallas, Houston, Austin and San Antonio. Similarly, the Atlanta metropolitan region in Georgia shows lower chronic disease rates compared to surrounding areas.
Areas with high chronic disease prevalence often share common socioeconomic characteristics. If you live in these areas, you’re more likely to face higher rates of disability, unemployment and reliance on government assistance programs like SNAP. Educational attainment is also a significant factor — areas with lower chronic disease prevalence have a much higher proportion of residents with post-high school education.
The economic divide is stark: the median income in areas with the lowest chronic disease prevalence is nearly double that of areas with the highest prevalence. Home values show an even more dramatic disparity, with median values in low-prevalence areas being almost three times higher than in high-prevalence areas.
These disparities highlight the profound impact that your local environment and community characteristics have on your health. Still, along with recognizing risks associated with your location, remember that it’s also important to take proactive steps to mitigate them.
The Psychic Health Crisis: A Hidden Epidemic Within the Chronic Disease Pandemic
While physical chronic diseases have been at the forefront of health discussions, psychic health disorders are rapidly becoming a significant part of the global disease burden. Psychic health issues account for 20% of the global disease burden, with addiction, mood disorders and anxiety playing major roles.
There’s often a delay in seeking treatment for these conditions. For instance, obsessive-compulsive disorder (OCD), one of the top 10 leading causes of disability in the developed world, typically goes untreated for about 10 years. Similarly, people with gambling disorder often wait around nine years before seeking help.
These delays significantly increase the burden of disease. Recognizing the importance of mental health in overall well-being is crucial for your health journey, as psychic and physical health are deeply interconnected.
Addressing the Four E’s to Prevent Premature Deaths from Chronic Disease
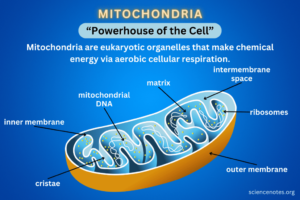
Optimizing mitochondrial health is the most important step you can take to achieve vibrant, lasting health and avoid chronic disease, as impaired mitochondrial function lies at the heart of most chronic conditions.
There are about 100,000 trillion mitochondria in your body, each with hundreds of electron transport chains. Their staggering numbers reveal just how vital they are to your cellular function and, by extension, your overall well-being. Your mitochondria produce adenosine triphosphate (ATP), which is critical for every function in your body. Without energy, your cells can’t repair and regenerate themselves.
The fundamental issue underlying most chronic disease is that your cells are not producing enough energy. There are four primary factors decimating your cellular energy production — the four E’s:
- Excess essential fats (seed oils) — The excess consumption of processed seed oils, which are prevalent in modern diets, particularly in processed foods, poses significant health risks. These oils, rich in linoleic acid (LA), severely impact your mitochondrial function.
- Estrogen — Estrogen increases intracellular calcium levels and decreases mitochondrial function. In fact, estrogen dominance is nearly as dangerous as excessive LA intake when it comes to destroying your mitochondrial function.
It’s important to minimize exposure to synthetic estrogens, such as those found in hormone replacement therapy and oral contraceptives. Xenoestrogens found in everyday items like plastic are another widespread source of exposure.
- Electromagnetic fields (EMFs) — The third significant threat to cellular health comes from the growing exposure to EMFs due to the proliferation of wireless technologies. EMFs increase calcium ion concentrations within cells, resulting in the production of harmful free radicals.
- Endocrine-disrupting chemicals (EDCs) — EDCs represent a broad category of substances, including plastics, that interfere with hormone function and have been linked to various health issues, including reproductive problems, developmental disorders and certain cancers.
These chemicals primarily work by activating estrogen receptors in your cells, similar to how EMFs activate voltage-gated calcium channels. This activation increases calcium influx into cells, and excess intracellular calcium dramatically increases superoxide and nitric oxide. These quickly combine to form peroxynitrite, which is an extremely potent oxidant stressor. This leads to severe oxidative stress and cellular damage.
Avoid Mitochondrial Poisons to Boost Your Cellular Health
These and other mitochondrial poisons lead to a disruption in the delicate oxygen balance within your gut, creating an environment that favors the proliferation of harmful, oxygen-tolerant microbes while inhibiting the growth of beneficial, oxygen-intolerant microbes crucial for gut health. Mucin acts as a binding agent for your colonic epithelium, with colonocytes forming a critical barrier.
When this barrier is compromised, it initiates a progressive decline in health, accelerating the aging process.
Addressing the underlying factors damaging colonocytes and restoring proper oxygen levels is essential for reestablishing the population of beneficial, oxygen-intolerant microbes. The communication between mitochondria and your gut microbiome is vital, but when oxygen-tolerant pathogenic bacteria predominate, they crowd out beneficial bacteria, impeding the production of necessary metabolites for optimal health.
Until excess oxygen is removed from your colon, even the most beneficial lifestyle factors such as exercise, sleep, nutrition and supplements may not lead to significant improvements. Simply introducing probiotics is not an effective solution, as commercially available probiotics are often non-viable in the gut environment. These may provide postbiotic benefits but cannot serve as true “seeds” to reestablish the proper microbial community.
Your gut environment needs to be healthy for oxygen-intolerant microbes to thrive, much like seeds require suitable conditions to grow. Avoiding mitochondrial poisons, like those above, is key to creating and maintaining this favorable environment for gut health and microbial balance, and ultimately for avoiding chronic disease.
Author: Dr. Joseph Mercola
yogaesoteric
December 11, 2024
