How Many of These Nine Factors Are Working Right Now to Wreck Your Gut Health?
The health of your microbiome depends on having the proper balance between beneficial bacteria and potentially pathogenic bacteria, as well as the health and integrity of your gut lining.
When your microbiome falls out of balance or loses its diversity, or your gut lining becomes compromised, it can impact many processes in your body and your risk of chronic disease.
Here are nine of the biggest factors:
Processed and sugary foods and pasteurized milk can harm your good gut bacteria
1. Antibiotics
Most antibiotics can alter your gut microbial balance. Whether you’re taking antibiotics right now, just finished a course last week or took them years ago, the well-being of your microbiome may be compromised. Included are the antibiotics hidden in food, especially factory-farmed meats and conventional dairy products.
2. Heartburn pills
A British study on twins suggests that proton pump inhibitors (PPIs) taken for heartburn can alter your gut flora. An additional 2015 study confirms differences observed in PPI users versus non-users are associated with changes towards a less healthy gut microbiome.
3. Fluoridated and chlorinated water
The chlorine in chlorinated tap water can potentially destroy both the bad bacteria and the good, friendly bacteria in your gut. The same is true for fluoride.
4. Processed and refined sugars
The chlorine in chlorinated tap water can potentially destroy both the bad bacteria and the good, friendly bacteria in One of the fastest ways to create an imbalance – and feed the bad guys – is to eat too much sugar and non-fiber carbohydrates. Few things fertilize and speed up the growth of pathogenic microbes faster than sugars!
5. Processed, refined foods
Processed foods, including pasteurized milk, can harm your good bacteria. Eating the typical Western diet of processed foods produces a profoundly different microbiome than one high in vegetables and fiber.
6. Bioengineered foods, pesticides and other agricultural chemicals
Certain genetically engineered foods and even some non-GMO foods that are not organic, like wheat, can contain glyphosate, an agricultural herbicide that’s been shown to target and destroy good gut bacteria. Conventionally raised animals are typically fed bioengineered grains, such as GE corn.
7. NSAIDs (Nonsteroidal anti-inflammatory drugs)
Certain popular over-the-counter painkillers can damage cell membranes and your gut lining, and harm healthy gut flora.
8. Stress
Stress affects your gut in a number of ways including hindering the production of enzymes and absorption of nutrients, and reducing oxygen levels and blood flow. Plus, it can impact the functioning of your entire GI tract, including your gut flora.
9. Pollution
Airborne particulate matter from car exhaust, home furnaces, and industry, as well as livestock emissions travel from your lungs to your intestines, and can alter your gut bacteria and your intestinal barrier. It can contaminate the food and water supply, leading to further injury of your gut bacteria.
Now that you know what can destroy or upset the balance of your microbiome and the integrity of your gut lining, let’s look at what you can do to help restore your gut health to support your health and well-being.
The Two “R’s” – and Why Your Microbiome Needs Them
A healthy microbiome contains two different types of bacteria. You get essential bacteria from your parents, but there’s another important source: your environment.
1. Bacteria from Mom (and Dad to a lesser degree) during the birthing process, breast-feeding and close interactions with friend and family shortly after birth. These include the commonly used probiotic species lactobacillus and Bifidobacterium. These organisms are essential for your body’s functioning and control its many biochemical reactions. The typical western lifestyle causes significant harm to these bacteria, which can lead to dysbiosis, or an imbalance of microbes.
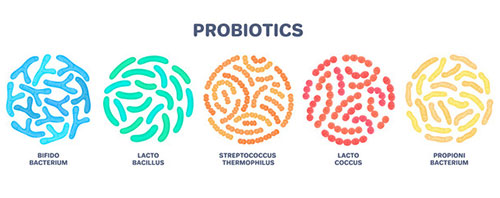
2. Transient organisms from the natural environment. These microbes are key “reconditioning” probiotics. They are introduced into your microbiome through environmental exposure in the form of spore organisms. These important bacteria perform critical housekeeping functions in your gut. They’re sometimes referred to as the “gut police” because they take care of the condition of your gut and support the growth of good bacteria.
Think of these two categories of bacteria as “reconditioning” and “reseeding.” Environmental bacterial spores condition your gut and ready it for reseeding by beneficial bacteria from fermented vegetables or probiotic supplements.
We’ve talked about how everyday living conditions and lifestyle can easily disrupt your delicate microbial balance and gut lining integrity. And we’ve explored how by avoiding dirt and focusing too much on sanitation, we sidestep and destroy the environmental organisms so crucial to your gut health.
Why Regular Probiotics May Not Be Enough to Support Your Gut Health
Mother Nature produces bacterial spores as a means to survive extreme environmental conditions and to exist long-term in conditions that might normally kill the bacteria. The complex spore-forming process takes about eight hours. It involves the buildup of layers surrounding the bacteria core, ending with outer protein-like layers known as the spore coat.
Different from regular probiotics, spore-forming bacteria offer four major advantages over non-spore-forming probiotics such as Lactobacillus in your gut:
– Spores can survive the low pH of your stomach to reach your small intestine intact;
– Spores can survive the low pH of the gastric barrier to deliver the entire dosage to your small intestine (not the case for all Lactobacillus species);
– Spores resist breakdown from enzymes, solvents, and hydrogen peroxide as they travel to your small intestine;
– Spores are heat-stable, so the product can be stored at room temperature without losing any potency or effectiveness;
– Certain spores are antibiotic-resistant, which means you can take them while using antibiotics to help support your healthy microbiome.
When the spores reach your small intestines and are exposed to the right nutrients, they germinate. This process, which takes just a few minutes, allows water to enter the spore and break down and remove the spore coats. Freed of its protective layers, the beneficial probiotics can resume cell growth inside your body.
Here’s what it’s important to keep in mind about spores and regular probiotics: They’re not interchangeable as they perform different functions in your gut.
To truly optimize the health of your microbiome, you need both!
Bacillus – Nature’s Original Spore Probiotic That Benefitted Even Dinosaurs?
Bacillus has been around for millions of years. Because our ancestors were hunters and gatherers and ate off the land, much of their diet was teeming with environmental bacteria. These strains of bacteria were able to survive in the outside environment, and they were able to pass through the acidic gastric system and end up thriving in the intestines.
After thousands of years of exposure, humans have actually come to require these specialized strains for proper, healthy function of many of our biological systems! The most well-known, well-studied and widely used spore probiotics are from the bacillus species – in particular bacillus subtilis, bacillus clausii and bacillus coagulans.
You won’t find these spore probiotics in foods, as our modern sterilized food systems have eliminated these critical species from our diets. So where can you find them?
Originally thought of as “soil organisms,” studies show they are actually digestive tract organisms that use the soil to transfer themselves from host to host.
Bacillus species are very abundant in the environment and data suggests they spanned the globe thousands of years ago. While bacteria are known to mutate very quickly, the bacillus subtilis species has remained the same for tens of thousands of years – proof of how resistant bacillus is as an environmental probiotic!
Bacillus species, including bacillus subtilis, bacillus clausii and bacillus coagulans have been shown in research to:
– Train the immune system to support a healthy normal inflammatory and immune response;
– Support digestion and assimilation of food and nutrients;
– Support detoxification processes of your GI tract;
– Support your GI defenses against invading species and bacterial overgrowth, including your small intestine;
– Produce key nutrients at the site of absorption to maximize bioavailability.
Bacillus spore probiotics produce vitamins, enzymes, carotenoid antioxidants, and some very valuable fats…
Short-Chain Fatty Acids – The MOST Important Nutrient for a Healthy Gut?
Do you have enough of these gut-loving fatty acids for your healthy microbiome?
Some researchers believe short-chain fatty acids (SCFAs) may be the most important nutrient for a healthy gut and microbiome.
SCFAs are fatty acids produced by your gut microbiota as fermentation products from unabsorbed food in your small intestine. What sets them apart from other fatty acids is their unique structure: Fewer than six carbons in straight and branched-chain configurations.
The most abundant SCFAs are acetic acid (C2), propionic acid (C3), and butyric acid (C4). They comprise as much as 95 percent of the SCFAs in your colon.
SCFAs play important roles in the health of your microbiome and gut:
– Support healthy blood flow and fluid and electrolyte uptake;
– Promotes healthy intestinal permeability, helps heal your gut and keeps your gut wall sealed;
– Promotes the production of immune cells;
– Increases fat metabolism;
– Supports the growth of beneficial organisms (lactobacillus and bifidobacter);
– Helps promote a healthy normal gut and systemic inflammatory response.
In recent years, propionic and butyric acids have received the most attention for a very good reason: Low levels of these are connected with inflammatory processes in your body.
The highest concentration of butyrate in your body is in your gut. This short-chain fatty acid is an important energy source for your intestinal cells. If levels of butyrate run low – or are diminished – intestinal cells die. Butyrate also plays key roles in supporting digestive health and a normal inflammatory response in your gut.
Diet does not provide a reliable, absorbable source of SCFAs, so you must depend on key gut bacteria to produce SCFAs (especially butyrate) for your microbiome.
yogaesoteric
January 27, 2020
