How your microbiome influences your immune system
Your immune system and gut microbiome share a symbiotic relationship and your immune function is largely dependent on the state of your gut. More than 99% of your genes come from microbes, not your chromosomes. The best predictor of future health is your gut microbiome at birth.
This article is part of a weekly series in which Dr. Mercola interviews various experts on a variety of health issues. In this interview, Rodney Dietert, Professor Emeritus of immunotoxicology at Cornell University, reviews the interrelationship between your immune system and your gut microbiome.
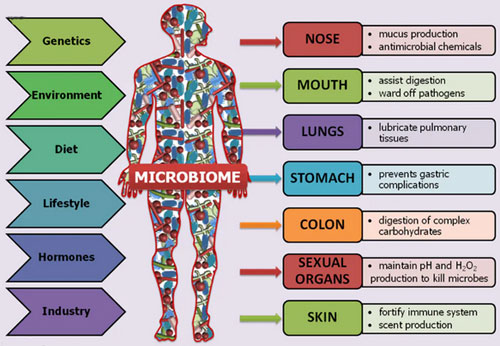
He’s spent several decades researching and teaching students about the immune system. As noted by Dietert, your gut microbiome is crucial not just for immune function, but also for your health status in general, as it affects nearly all other physiological systems.
He first became aware of the importance of the gut when given the opportunity to write a research paper about which biomarker would be the best to predict the future health of a baby.
“I thought that was a really intriguing question to develop a paper around,” he says. “And, I was pretty sure decades of work on the immune system in the young, prenatal and neonatal, meant that I had an answer. I became very frustrated because I wrote a couple of paragraphs and it was unpersuasive, and went to bed extremely frustrated. I woke up in the middle of the night from a dream with what to me was an answer.
The answer was that it was the extent to which the newborn became complete or completed itself, and that that self-completion is really the installation of the microbiome, largely from the mother, but both parents contributing; vaginal delivery when possible, skin-skin contact, and then of course, followed up with prolonged breastfeeding when possible.”
Ancestral microbiomes
He points out that “more than 99% of your genes are from microbes, not from your chromosomes.” You have approximately 3.3 million microbial genes, mainly bacterial. Across the entire population of humans, there are just under 10 million different microbial genes, so you won’t necessarily have all of them. You also have 22,000 to 25,000 chromosomal genes (these genes are what were analyzed through the Human Genome Project), which means you only have about 2,000 more chromosomal genes than an earthworm. As noted by Dietert, since we have about 3.3 million microbial genes, that means we’re more than 99% microbial, genetically.
This is why he concluded that the gut microbiome at birth would be the best predictor of future health. Granted, your microbiome can be altered through diet and environmental exposures, and that will impact and influence your health throughout your life. But initially, the infant microbiome is the best overall predictor of future health. “That led to a whole host of other lectures, books, scientific journal articles and an appearance in the documentary movie, ‘MicroBirth,’ which is a wonderful film. It won the life science award in 2014 for documentary films. That launched a second career, really, as a result of a dream, and paying attention to that versus the linear progression of 30-plus years of research.”
According to Dietert, there’s really no single measure of any particular bacterial species that will give you a definitive answer to what your health will be like. Rather, the most important predictive aspect is the seeding process. If the baby goes through an ideal seeding process at birth, he or she stands a greater chance of experiencing good health.
“Healthy microbiomes are more connected to what your ancestors had that has been lost through short-sighted practices and technology installations. Trying to head toward that is much more constructive than trying to completely overhaul something to a group of microbes your ancestors never saw” – Rodney Dietert.
For example, elective cesarean and antibiotic regimens – both in the mother and the baby – are known to degrade the baby’s microbiome. Since 2012, when he had that dream, he’s been able to map out more specifics, but there’s no single ideal microbiome per se. There are many different healthy microbiomes. “These [microbiomes] arose in our ancestors depending on their geography, diet and a whole host of factors that were honed over thousands of years,” he explains.
“For example, I have in my 60s tried to modify my health constructively by modifying my microbiome, and in my case, it would’ve been a long reach to get an ideal Asian microbiome because that’s not really my ancestry. It’s not where I grew up, or the soil I lived on and the food I ate.
So, healthy microbiomes are more connected to what your ancestors had that has been lost through short-sighted practices and technology installations. Trying to head toward that is much more constructive than trying to completely overhaul something to a group of microbes your ancestors never saw.”
Compensatory practices
Past dogma stated that the infant’s immune system was complete at birth with little to no maturation or adjustment required in the infant. Now we realize that this is not true. The baby’s immune development in utero is not uniform. It is skewed to protect maintenance of the pregnancy. This skewing then needs to be adjusted in the newborn/infant and the immune system must be expanded, redistributed, and rebalanced.
The best way to do this is by ensuring that rebalancing the baby’s microbiome is complete and that a healthy infant microbiome can drive necessary post-natal immune maturation. If microbially-driven, infant immune maturation does not happen, then immune dysfunction-driven disease is an increased likelihood for that child. Remember that 60% to 70% of your immune cells are located in your gut and these immune cells are in close proximity to your gut microbiome. So, gut microbiome status and immune status are intimately intertwined.
As mentioned, having a C-section puts your newborn at serious risk for developing a less than optimal microbial population. However, in some cases, a C-section is necessary, and the good news is you can compensate for the loss of microbial seeding that would have occurred during vaginal birth. Gloria Dominguez Bello, Ph.D., at Rutgers University, who has pioneered much of this work, uses a vaginal swab technique where the microbes from the mother’s vagina are manually transferred to the baby immediately after birth. You can learn more about this technique in “The Importance of Reducing Your Toxic Burden When Planning to Start a Family.” “While it’s not 100% equivalent, it is very good,” Dietert says.
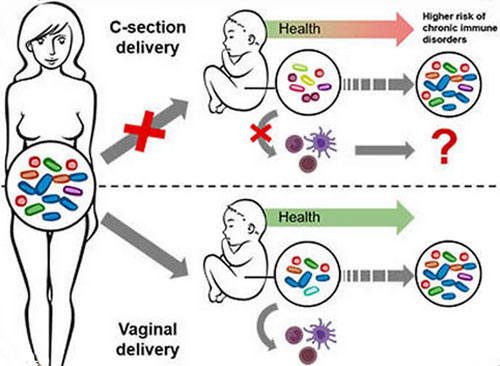
“Those types of strategies are the direction we need to head in to really aid parents in being able to deliver the majority of the baby’s genetics. Those microbial genes are making proteins and enzymes, they’re modifying what we see from the external environment, they’re modifying our diet [via microbial metabolism] before our mammalian human cells ever see anything. In effect, if you look at interference with seeding the [baby’s complete] microbiome, to me, that is like a birth defect. If you were missing an organ or a limb, that would be a birth defect. Here, you’re missing the majority of your genetics [the microbiome as a virtual organ containing most of the baby’s genes].
Yet, that is a correctable birth defect and we need to keep that in mind. That would really be the push and the goal – to ensure the baby is able to have, as soon after birth as possible, the robust microbiome that would normally be there…
We know from experience that status of the microbiome dramatically impacts aspects like risk of asthma at age 7, and then subsequent health risks as well. Even picking up atherosclerosis markers, which you now can measure in children even though the disease onset will probably be decades off…
If you’re growing up on a farm and having raw milk, and are exposed to animals and the microbes that go with that environment, it turns out that’s rather protective against asthma and allergy later in childhood, as long as you’re not directly encountering pesticides. That [encountering pesticides] will eliminate the benefit [of the early life microbial exposures].
Those microbial exposures early in life are really what our ancestors had to develop an appropriately balanced immune system, a well-regulated immune system. If we don’t do that, then you’re shifted toward a proinflammatory state and your regulation of immunity is off [producing an increased risk of later-life diseases].
Nature tells us that the microbiome has to have some compatibility with the immune system as they co-mature. When you get microbiomes that are really foreign to an immune system, the immune system [rather than developing self-tolerance] responds with a massive inflammatory response, so there’s a self-attack …”
Aside from the vaginal tract, the baby also receives valuable microbes via skin-to-skin contact, including oral contact with breast tissue, as well as from the breast milk itself, which is why breastfeeding is so important and can impact your child’s health well into the future. As mentioned above, environmental exposures from soil, food and animals also play a role.
Epigenetic interactions
Your microbiome (in addition to directly metabolizing your food, drugs and chemicals) also influences the epigenetic expression of your (chromosomal) genes. For example, Dietert cites the work of Curtis Klaassen, former president of the Society of Toxicology and an expert on liver metabolism, who years ago shifted focus to microbiome metabolism because, epigenetically, microbes influence liver metabolism.
“The microbes [encounter and respond to] our food first. They see our environmental chemicals first. They see drugs through most routes of administration first, and what they do with those determine what your body sees. So, they’re our gatekeeper, they’re our filter for our whole environmental existence.
As a result, it’s important to know what happens there. An example is cancer therapeutics. Most of those have to be metabolized by the microbiome. If we manage the microbiome more effectively in patients, we very likely could increase the efficacy of those drugs across a population of patients.
I think the U.K. said they’re about 50% effective. That could be increased because we’ve ignored the microbiome and its role, even though these drugs don’t work unless they’re metabolized by the microbiome. [We now have more capability to manage microbial metabolism and should be doing that as part of sustainable health care.]”
How your gut microbiome impacts immunosenescence
Historically, the thymus gland has been known to be really important for the development of the immune system, and in older individuals, the deterioration of the immune system is frequently related to thymic deterioration. The good news is this can to some extent be compensated for by improving your gut microbiome. Dietert explains: “Aging of the immune system is really dependent upon your lifetime diet in large part. So, you don’t have to buy into the fact that there is only one end for an 80-year-old’s immune system – senescence, lower responses to certain infectious disease agents and greater risk of auto-reactivity. You really don’t have to buy that, because it is largely influenced by diet and microbial metabolism.”
One factor that plays a significant role in the destruction of your gut microbiome is the use of medications. According to Dietert, 25% to 50% of all drugs, including over-the-counter medications, damage your microbiome in predictable ways. Other drugs interact with the microbiome modifying drug treatment outcomes. We ignore these drug-microbiome interactions at our own peril. “For example, here’s just one case that’s historic: Digoxin, a long-standing heart medication, can be metabolized by one specific bacterial species [Eggerthella lenta]. Now, depending on the level of that [specific bacterial] species that you have in your gut, the drug will either be ineffective because of the metabolic level, it will be effective, or it will be toxic and kill the patient. It’s a bit of a problem in terms of prescribing [a safe and effective personalized dose of Digoxin], even though it can be an effective drug.
Knowing that [the drug-microbiome relationship], and knowing it’s one specific [gut] bacterium [controlling internal drug dose], which could be measured, [the bacterium] could be supplemented and the level [of bacterial metabolism of Digoxin] could be modified or the[administered] drug level could be modified [to ensure that drug metabolization by the gut microbome results in a safe and effective internal dose for each individual]. Why wouldn’t you do that if you were going to administer this type of drug? [The microbiome and therapeutic drug dose can and should be aligned in each patient].”
So, the more microbe-damaging drugs you use, the greater the degradation of your microbiome will be over time. When combined with a poor diet, you end up with immunosenescence – the gradual deterioration of your immune system – but it’s not a given just because you get old if you protect and support your microbiome and immune system across the life span. “As always when you’re dealing with the immune system and inflammation, it’s a matter of tissue integrity and the question of whether you’ve so damaged an organ that it’s going to be tough to come back from,” Dietert says. “You want to make these [inflammation-controlling] corrections [in your microbiome and immune system] before [a point of no return when] you’ve completely lost good [tissue] function due to massive inflammatory damage over decades.”
Avoid unnecessary antibiotic exposure
One simple strategy that will protect your microbiome is to avoid antibiotics. While they may be necessary to combat an active infection, the vast majority of antibiotics you’re exposed to come from food. Animals raised in concentrated animal feeding operations (CAFOs) are routinely fed antibiotics that you then ingest when you eat that animal.
That’s one of the reasons why there is a strongly support and recommendation of eating organic, as organically raised animals are not allowed to be given antibiotics unless the animal is actually ill. CAFO animals are also more prone to carry antibiotic-resistant bacteria.
The COVID-19 pandemic has also increased the use of antibacterial products. People think they’re killing harmful germs but, in reality, they’re just killing their immune system. As explained by Dietert: “Is necessary for you to support your entire body and to support your immune system as well. I’d point out that, for example, glyphosate is an antimicrobial. First, it destroys soil microbes, then plant microbes, and then it gets into animals and into us. We’re exposed directly and we’re exposed through food.
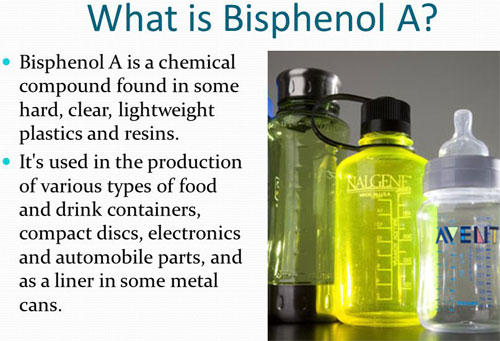
Again, it’s widespread and it’s just one example. You can take the plasticizers, bisphenol-A and others, where these aspects were never screened properly and the attention to the microbiome was never given. That’s a huge mistake and we need to reverse that immediately.
I’m a big proponent of regenerative agriculture … I look at ecological management of microbes and robust diversity of plants, animals and our food production as critical. I’d like to point out that COVID-19 is in fact a cytokine storm.
It is an improper host immune response that leads to lung pathology and increased risk of death. Yet there’s been almost no attention paid to the multiple factors that influence the immune system, inflammation and what’s called ‘colonization resistance.“
Colonization resistance
As explained by Dietert, you carry coronaviruses in your airways. Most have some coronavirus in the airway, but it won’t cause illness as long as you have a healthy airway microbiome. A healthy airway microbiome is supported and promoted by aspects like physical exercise and spending time outdoors where sun exposure will optimize your vitamin D level. “To grow our own food, get outside, visit animal farms and have microbial exposures in a healthy way, increase our vitamin D and tend to our immune system and our overall health is absolutely critical,” he says.
“The more robust the microbiome [along with production of anti-pathogen metabolites], the better the colonization resistance we have against these pathogens. [This includes protection against] the secondary bacterial infections that will [frequently] arise during the mix of modifying a [healthy] lung environment [to one engulfed in a] pro-inflammatory state.
We should’ve been doing that from the word go but, unfortunately, we have some scientists and bureaucrats that focused in one place and didn’t really focus, in my opinion, on human health.”
As just one example of how healthy bacteria can prevent infection, Lactobacillus acidophilus has been shown to block salmonella infection and spread in chickens. In the early 1990s, this type of intervention actually ended up saving the poultry industry that was having a massive salmonella problem, yet you never hear about that.
“I think this shows we need to manage how we produce our food. We need to recognize the benefits of a variety of supplements. I think that is what’s going to help get us out of the polypharmacy rut that we’ve been in, quite frankly.”
It’s really a classic example of competitive inhibition, and it works the same way in the human body. According to Dietert, as few as 15 beneficial bacteria are able to create a metabolic environment in the gut that keeps the salmonella bacterium in check, thereby preventing it from multiplying out of control and causing disease.
So, with a robust diversity of beneficial bacteria in your gut, you’re effectively able to block infection from occurring even though you may be exposed to dangerous pathogens. Keep in mind that the composition of your microbiome will also play a significant role in how well you can handle dietary “cheating” or the occasional junk food indulgence. As noted by Dietert: “If you have a particularly robust microbiome, you’re probably more resilient to a junk food weekend. If you are already dysbiotic or you’re weakened in your microbiome because of chronic conditions, polypharmacy or glyphosate exposures, then you probably are pretty vulnerable to further shifts. Again, it’s how well are you seeded with a robust diversity? It’s like forest management in ecology or coral reef management. If you’ve got a coral reef that’s already damaged and sick, then it isn’t going to take much to really put it over the top in terms of serious changes. This would be the same for us in terms of immune inflammation, pathology and/or an infectious agent getting a foothold, whereas it wouldn’t otherwise.”
From gut to brain
One way by which beneficial bacteria protect your health is through the production of butyrate and mucin, the mucous layer that protects the intestine. Gut microbes also make neuroactive peptides and neurotransmitters. There’s a whole field that’s been developed called psychobiotics that focus on using bacteria for neurological and mental health.
“Certain bacterial species and strains will produce serotonin, for example. Others produce dopamine. Some produce GABA or acetylcholine. While most of the neurotransmitters produced in the gut cannot penetrate the blood-brain barrier, and therefore will not increase levels in the brain directly, they still have an indirect and measurable effect”, Dietert says. The vagus nerve is one path through which the gut microbes influence brain chemistry and physiology.
How to address leaky gut
Leaky gut is now recognized by most conventional physicians as a condition that contributes to other pathologies and chronic diseases. One important strategy to address leaky gut is to optimize your vitamin D, as it helps regulate your innate immune system and increases your body’s ability to repair epithelial cell damage and gaps in the intestinal barrier.
Dietert also recommends supplementing with keystone species bacteria such as the genus Akkermansia, which is involved with mucin regulation. There are only a couple of bacteria that do that. He stresses that while vitamin D is important for gut repair, you also need bacteria to help maintain the mucin layer, as this is what keeps inflammatory bacteria and particles from seeping through the intestinal barrier.
Baking soda (sodium bicarbonate) or potassium bicarbonate can also be very helpful. Is preferable, in many cases, potassium bicarb because most of us have excess sodium and not enough potassium. We can take about a half a teaspoon of potassium bicarb three times a day. We can use a urinary pH to monitor and adjust the dosage. The urine pH should be about 7, which is neutral. This will also help prevent the leaching of minerals from bones.
Your health begins in your gut
In closing, Dietert reminds and encourages us to “do actions that support your whole body, do actions that support your immune system, even as you’re focused on a specific disease or a specific pathogen.” The reason for doing this is because everything is connected.
“We’re now realizing that the boundary between infectious or communicable diseases and noncommunicable diseases may not be as rigid as we used to think,” Dietert says. “People have been able to show that if you install the wrong microbe into your gut microbiome – one that’s dysfunctional and not very robust – you can wind up with a predictably-increased risk of very specific noncommunicable or chronic diseases. We never thought that was the case, but there’s evidence emerging, really within the last couple of years, that [chronic diseases] are all about microbial management. So, understanding your body, understanding your genetics and taking advantage of that, [can allow you] to be naturally healthy.”
