Nutritional deficiency causes most disease (2)
Read the first part of the article
- Depression
Depression leads to hair loss, rashes and mental issues which are caused by the deficiency of Vitamin B7. It can be prevented by eating diary properties, peanuts and other sources of vitamin.

Biotin, also called vitamin B7, is involved in a wide range of metabolic processes, both in humans and in other organisms, primarily related to the utilization of fats, carbohydrates, and amino acids. The name biotin derives from the Greek word “bios” (“life”) and the suffix “-in” (a general chemical suffix used in organic chemistry)
The biotin recommended daily intake (RDI) for both males and females are: 5 μg/day of biotin for 0-to-6-month-olds, 6 μg/day of biotin for 7-to-12-month-olds, 8 μg/day of biotin for 1-to-3-year-olds, 12 μg/day of biotin for 4-to-8-year-olds, 20 μg/day of biotin for 9-to-13-year-olds, 25 μg/day of biotin for 14-to-18-year-olds, and 30 μg/day of biotin for those 19 years old and older. The biotin RDI for females who are either pregnant or lactating, respectively, are: 30 μg/day of biotin for pregnant females 14-to-50-years old and 35 μg/day of biotin for lactating females 14-to-50-years old. The European Food Safety Authority (EFSA) also identifies RDI setting values at 40 μg/day for adults, pregnancy at 40 μg/day, and breastfeeding at 45 μg/day. For children ages 1-17 years, the RDI increase with age from 20 to 35 μg/day.
Factors that affect biotin levels are: chronic alcohol use, anti-epilepsy drugs carbamazepine and primidone, partial gastrectomy or other causes of achlorhydria, burn patients, age (elderly individuals) and sport (athletes). Pregnancy and lactation may be associated with an increased demand for biotin.
Primary biotin deficiency, meaning deficiency as a consequence of too little biotin in the diet, is rare, because biotin is contained in so many foods. Subclinical deficiency can cause mild symptoms, such as hair thinning, brittle fingernails, or skin rash, typically on the face.
Aside from inadequate dietary intake (rare), deficiency of biotin can be caused by a genetic disorder that affects biotin metabolism. The most common among these is biotinidase deficiency. Low activity of this enzyme causes a failure to recycle biotin from biocytin. Treatment is lifelong dietary supplement with biotin
– Correcting the deficiency:
| Source | Amount (μg / 100 g) |
Source | Amount (μg / 100 g) |
| Eggs | 21 | Peanuts, roasted | 17.5 |
| Egg white | 5.8 | Sunflower seeds, roasted | 7.8 |
| Egg yolk | 27 | Almonds, roasted | 4.4 |
| Cheese | 1.4 | Sweet potato | 1.5 |
| Milk | 0.1 | Broccoli | 0.9 |
| Bread | 0.1 | Tomato | 0.7 |
| Oatmeal | 0.1 | Strawberry | 1.5 |
| French fries | 0.3 | Avocado | 1.0 |
| Potatoes, mashed | 0.1 | Corn, canned | 0.05 |
| Corn flakes cereal | 0.1 |
8. Marasmus
Marasmus is a severe form of malnutrition, where we can find severe nutritional deficiency in number of proteins and minerals. It even leads to dry skin, loose skin folds, infections, loss of fluids and circulation disorders.
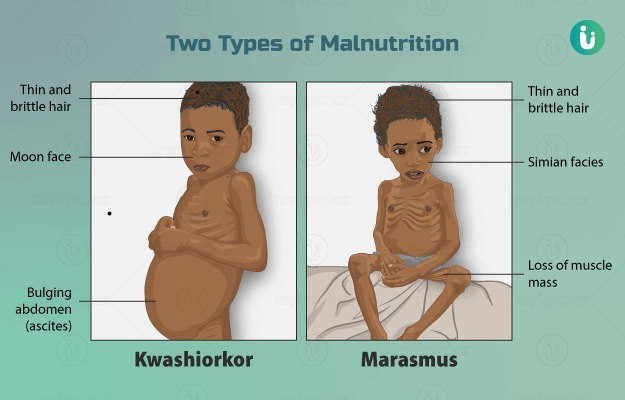
Marasmus is a form of severe malnutrition characterized by energy deficiency. It can occur in anyone with severe malnutrition but usually occurs in children. Body weight is reduced to less than 62% of the normal (expected) body weight for the age. Marasmus occurrence increases prior to age 1, whereas kwashiorkor occurrence increases after 18 months. It can be distinguished from kwashiorkor in that kwashiorkor is protein deficiency with adequate energy intake whereas marasmus is inadequate energy intake in all forms, including protein. This clear-cut separation of marasmus and kwashiorkor is however not always clinically evident as kwashiorkor is often seen in a context of insufficient caloric intake, and mixed clinical pictures, called marasmic kwashiorkor, are possible. Protein wasting in kwashiorkor generally leads to edema and ascites, while muscular wasting and loss of subcutaneous fat are the main clinical signs of marasmus. The prognosis is better than it is for kwashiorkor but half of severely malnourished children die due to unavailability of adequate treatment.
The word “marasmus” comes from the Greek μαρασμός marasmos (“withering”).
Marasmus is caused by maternal malnutrition, maternal anemia, poverty, pathological conditions in a baby (e.g., diarrhea), pneumonia, cyanotic heart diseases, malaria, necrotizing enterocolitis, pyloric stenosis, lactose intolerance, intussusception, meningitis or anorexia nervosa.
- Kwashiorkor
This is caused by lack of protein and energy in body. It is characterized by an enlarged liver, irritability and ulcerating dermatoses. It is also caused by malnutrition. A healthy and balanced diet with proteins and carbohydrates like eggs, lentils, rice will help to get rid of this problem.
Recent studies have found that a lack of antioxidant micronutrients such as β-carotene, lycopene, other carotenoids, and vitamin C as well as the presence of aflatoxins may play a role in the development of the disease. However, the exact cause of kwashiorkor is still unknown. Kwashiorkor is one of the main forms of childhood malnutrition living in low-income and middle-income countries. Kwashiorkor is oftentimes referred to as severe acute malnutrition (SAM).
Inadequate food supply is correlated with occurrences of kwashiorkor; occurrences in high income countries are rare. It occurs amongst weaning children to ages of about five years old.
Both kwashiorkor and marasmus fall under the umbrella of deficiencies called Protein Energy Malnutrition (PEM). These diseases are oftentimes discussed together, but can be distinguished. Kwashiorkor is classified by its insufficient protein consumption whereas marasmus is related to general energy deficiency and severe muscle wasting. Kwashiorkor is also distinguished from marasmus by the presence of edema. There is also marasmic kwashiorkor that is the deficiency of both calories and proteins. Although they are both different types of severe acute malnutrition, there was greater consumption of antioxidants, vitamins, and minerals seen in those with kwashiorkor compared to those with marasmus.
- Osteoporosis
This is caused due to lack of vitamin D in your body. Deficiency of vitamin D and calcium leads to unhealthy soft and brittle bones that are prone to fracture and defects in the spine structures. The term osteoporosis refers to the ‘porous’ (spongy) state of bone that eventually manifests as the bone’s ability to replenish itself declines over time. When persons reach the age of around 40, the rate of bone breakdown starts to exceed the rate at which it is replaced, creating increasingly larger holes in the bone that make it less dense and more prone to fracture.
Osteoporosis is a progressive metabolic bone disease that causes a decrease in bone density and gives rise to weak, fragile bones that are prone to fracture. Most commonly, these fractures occur in the spine, wrist and hips when a person falls or bumps into something. If such an event triggers a visit to the doctor, a test of the bone mineral density called a DEXA scan may be performed and reveal osteoporosis.
Vitamin D is important for the absorption of minerals such as calcium and phosphorus in the body. The minerals are absorbed from ingested food and supplements and deposited in the bones.
Vitamin D has been referred to as the “sunshine vitamin,” as skin exposure to sunlight is required to convert a precursor of vitamin D found in food sources to a form of vitamin D that can be used by the body. Cutaneous synthesis provides approximately 80% of the required vitamin D to the body. However if sunlight exposure is limited (as occurs in especially cold regions during wintertime), there is increased dependency on dietary sources to achieve necessary vitamin levels.
Calcium plays an important role in maintaining bone architecture, but is also required for regulating other functions such as blood coagulation, heart contractility, and neuromuscular activity.
– Calcium
Men and women between the ages of 18 and 50 need 1,000 milligrams of calcium a day. This daily amount increases to 1,200 milligrams when women turn 50 and men turn 70. The Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine recommends that total calcium intake, from supplements and diet combined, should be no more than 2,000 milligrams daily for people older than 50.

Good sources of calcium include: low-fat dairy products, dark green leafy vegetables, soy products, such as tofu, calcium-fortified cereals and orange juice.
If you find it difficult to get enough calcium from your diet, consider taking calcium supplements. However, too much calcium has been linked to kidney stones. Although yet unclear, some experts suggest that too much calcium, especially in supplements, can increase the risk of heart disease.
– Vitamin D
Most people need at least 600 international units (IU) of vitamin D a day. That recommendation increases to 800 IU a day after age 70. People without other sources of vitamin D and especially with limited sun exposure might need a supplement. Most multivitamin products contain between 600 and 800 IU of vitamin D. Up to 4,000 IU of vitamin D a day is safe for most people.
Dietary sources of vitamin D and calcium:
– Milk and dairy products, such as cheese (particularly ricotta cheese) and yogurt, are rich in both vitamin D and calcium. However, dairy products also tend to be high in fat, so they should be used in moderation as part of a balanced diet to prevent unnecessary weight gain.
-Egg yolks – Per the United States Department of Agriculture (USDA), a large egg, weighing approximately 50 g, contains approximately 50 IU of vitamin D3, with the largest concentration of calcium in the yolk. Including whole eggs in one’s diet can help increase vitamin D intake.
– Mushrooms – Cultivated mushrooms contain the plant ergosterol, which is a vitamin D precursor. When mushrooms are exposed to sunlight; they naturally produce vitamin D.
– Vegetables: Dark green vegetables like kale, spinach, okra, and collards are rich in calcium. These vegetables are an important component of vegan diets, which do not include animal-based foods.
– Banana and soy are also rich sources of vitamin D and calcium.
– Exercise
Good nutrition and regular exercise are essential for keeping your bones healthy throughout your life. Exercise can help you build strong bones and slow bone loss. Exercise will benefit your bones no matter when you start, but you’ll gain the most benefits if you start exercising regularly when you’re young and continue to exercise throughout your life.
Combine strength training exercises with weight-bearing and balance exercises. Strength training helps strengthen muscles and bones in your arms and upper spine. Weight-bearing exercises – such as walking, jogging, running, stair climbing – affect mainly the bones in your legs, hips and lower spine. Balance exercises such as tai chi can reduce your risk of falling especially as you get older.
Final words
Your body requires good quality food, meaning food that contains vitamins, minerals, proteins, carbohydrates and fats, food which is free of GMOs, pesticides and heavy metals. A balanced diet provide healthy nutrients for a good biology of the organism, and an adequate lifestyle provide regular exercise for an excellent tonus of the body.
yogaesoteric
February 12, 2022
