Woman’s Brain Inflammation Caused by Moderna Covid Vaccine, Authors of Case Study Conclude
A healthy 35-year-old woman who experienced a seizure two days after her second dose of Moderna’s covid-19 vaccine was diagnosed with limbic encephalitis, a rare form of brain inflammation.
The authors of a recent case study on the patient stated:
“We believe that this episode of limbic encephalitis, which occurred quickly after covid-19 vaccination, is an uncommon side effect of the [Moderna] vaccine.”
Limbic encephalitis is an acute condition of noninfectious inflammation of the brain that affects the limbic system.
The limbic system is a group of structures involved in processing emotion and memory. It includes the hippocampus, medial temporal lobe, cingulate cortex and frontonasal cortex.
The symptoms of limbic encephalitis include amnesia (memory loss), behavioral changes, psychiatric symptoms, seizures and a disturbed level of consciousness.
The pathophysiology (functional changes that accompany a particular syndrome or disease) of limbic encephalitis is known to be mediated (indirectly caused) by an antigen that stimulates an antibody-mediated host immune response that inadvertently targets cells in the limbic area.
There are two causes of limbic encephalitis: paraneoplastic and autoimmune.
“Paraneoplastic” means “caused by or resulting from the presence of cancer in the body but not the physical presence of cancerous tissue in the part or organ affected.”
The patient was screened for tumors, and cancer was ruled out as the cause in this patient’s case.
Case report
According to the case report, when the woman arrived at the hospital she had a fever, followed by generalized tonic-clonic seizures (formerly known as grand mal seizures) that lasted for approximately five minutes and a postictal (post-seizure) phase of confusion that lasted approximately 30 minutes.
During her stay in the emergency department, she had two more generalized seizures, which were controlled with medication, each one lasting less than two minutes after intervention.
The patient, who did not have any other neurological symptoms and was stable, was admitted to the hospital.
The authors wrote, “Apart from looking tired, she was oriented to time, place and person. Her neck was supported, and she had full power and sensation with normal higher functions. Cranial nerves were intact.”
The patient had a full basic blood workup, which was normal. Her covid-19 PCR test was negative. There was nothing unusual about her contrast MRI, performed upon her admission.
A lumbar puncture was performed, and her cerebrospinal fluid did have significant lymphocytosis — an abnormal increase in the number of lymphocytes (white blood cells), usually resulting from infection or inflammation.
During her hospital stay, the woman developed anisocoria, a condition in which the pupil of one eye differs in size from the pupil of the other eye. An urgent CT scan of the head showed possible temporal lobe hypodensities (darker areas on the CT scan).

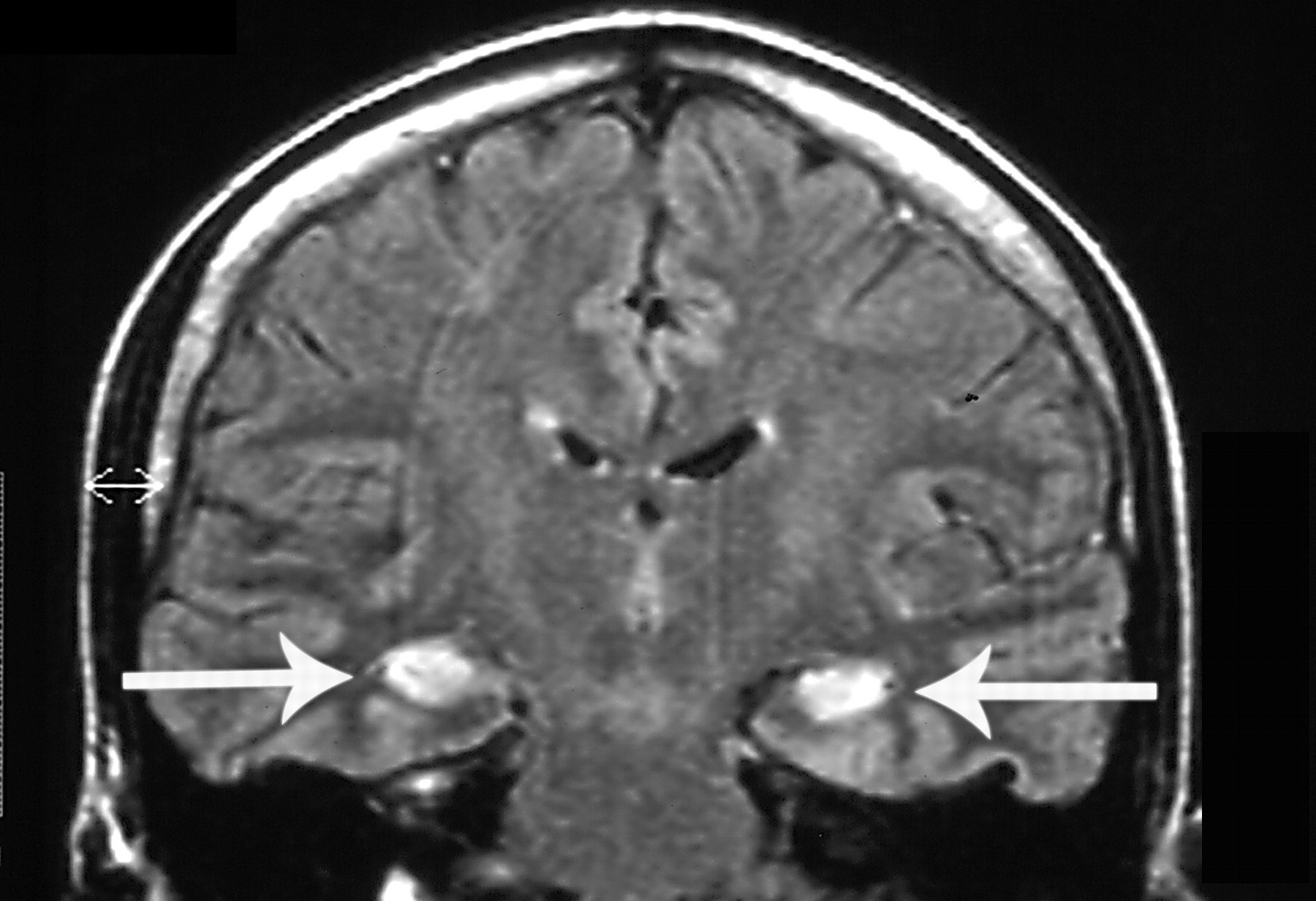
After discussion with the radiologist, the patient agreed to repeat the head MRI, which this time showed features suggestive of limbic encephalitis. A subsequent electroencephalogram showed severe post-seizure encephalitic changes.
Meanwhile, the results of the immunology screen became available and showed the patient was positive for antinuclear antibodies.
Antibodies are proteins that the immune system makes to fight foreign substances, such as viruses and bacteria. But an antinuclear antibody attacks a person’s own healthy cells instead. It is called an “antinuclear” antibody because it targets the cell nucleus.
Immediately after the positive antinuclear antibody test, the neurology team assessed the patient and started her on steroids, IV immunoglobulin and rituximab, a monoclonal antibody.
They “planned for a repeat lumbar puncture to check for autoimmune encephalitis, which unfortunately was not done due to financial issues,” the authors said.
While the patient was still in hospital, she developed abnormal behavior: agitation, abnormal laughing and crying. These symptoms are well-known to be associated with limbic encephalitis. The symptoms improved later with therapy.
The patient was diagnosed with autoimmune limbic encephalitis that caused the seizures based on her clinical presentation, imaging tests and the lumbar puncture finding.
The paraneoplastic type of limbic encephalitis was ruled out since no malignancy was found by CT scan and PET scan.
The patient’s symptoms improved and she was transferred to a rehabilitation facility to achieve full recovery. “Neuroimaging follow-up showed improvement and resolution of the previous limbic encephalitis changes,” the authors wrote.
According to the authors, “A complex set of investigations is required before the official diagnosis” of autoimmune limbic encephalitis. They noted there have been other documented cases of limbic encephalitis after vaccination.
The authors noted the patient’s limbic encephalitis occurred shortly after the second dose of Moderna, indicating a “temporal relationship between vaccination and symptom start,” similar to that reported in a study about series of cases of encephalitis after vaccination with AstraZeneca’s covid-19 vaccine.
It is not yet known what the pathophysiology of vaccine-related encephalitis could be, “but vaccines are well known for triggering the generation of pro-inflammatory cytokines and T-cell response,” the authors wrote.
According to the report, “Antigens will be recognized as possible pathogens by the immune system after immunization.” The subsequent inflammation could cause systemic side effects and, in rare cases, inflammation of the brain.
The authors concluded:
“We believe that this episode of limbic encephalitis, which occurred quickly after covid-19 vaccination, is an uncommon side effect of the vaccine. Our theory is based mainly on the timing of the symptoms, which began a few days after the immunization and in the absence of another identifiable cause.”
They added:
“The patient had an immune system-activating immunization and experienced an unusual autoimmune reaction shortly afterward. There is, however, some skepticism, mainly because the patient’s symptoms and signs have yet to be appropriately linked to a cause.”
yogaesoteric
November 6, 2022
